Every Saturday, about 40 people gather at a youth center in Mekelle to hear about a subject they don’t get taught in schools in Ethiopia, and don’t want to discuss with their parents – sexual and reproductive health (SRH).
This youth center located in the Tigray region of northern Ethiopia, is run by the Family Guidance Association of Ethiopia (FGAE) – it has a playground and library at the front for studying and socializing. In the back, there is a clinic and offices where staff provide a full range of SRH services, including free contraceptives, abortion care and testing and counselling for sexually transmitted diseases (STIs).
“In our country, we have a huge amount of youth and adolescents and it is very important to work with them on sexual and reproductive health,” said Mebrahtu Abadi, who manages this center in Mekelle, the capital of Ethiopia’s Tigray region.
Young people at the heart of the center
Ethiopia has Africa’s second largest population and according to government studies, youth makes up roughly a third of its population.
The center is aimed at people aged between 10 and 24 years old and runs a range of activities, including holding sessions in schools to bring people in for talks and services. On Saturdays, groups of young people usually do some performance art based on a particular SRH subject, and hold debates and discussions around a coffee ceremony – a traditional Ethiopian social gathering.
“In these ceremonies we prepare a poem or a short drama to entertain and educate using peer to peer methods about things like HIV and other sexually transmitted diseases, contraceptives, unplanned pregnancy and abortion”, said Abadi.
The youth center has 20 peer educators – 10 male and 10 female – who provide counselling to others at the center, in schools and communities. Tigray is home to about five million people and Mekelle is a large university town, so the centre also works with campus clinics and with university and school clubs focusing on sexual health education.
Peer educators leading the change
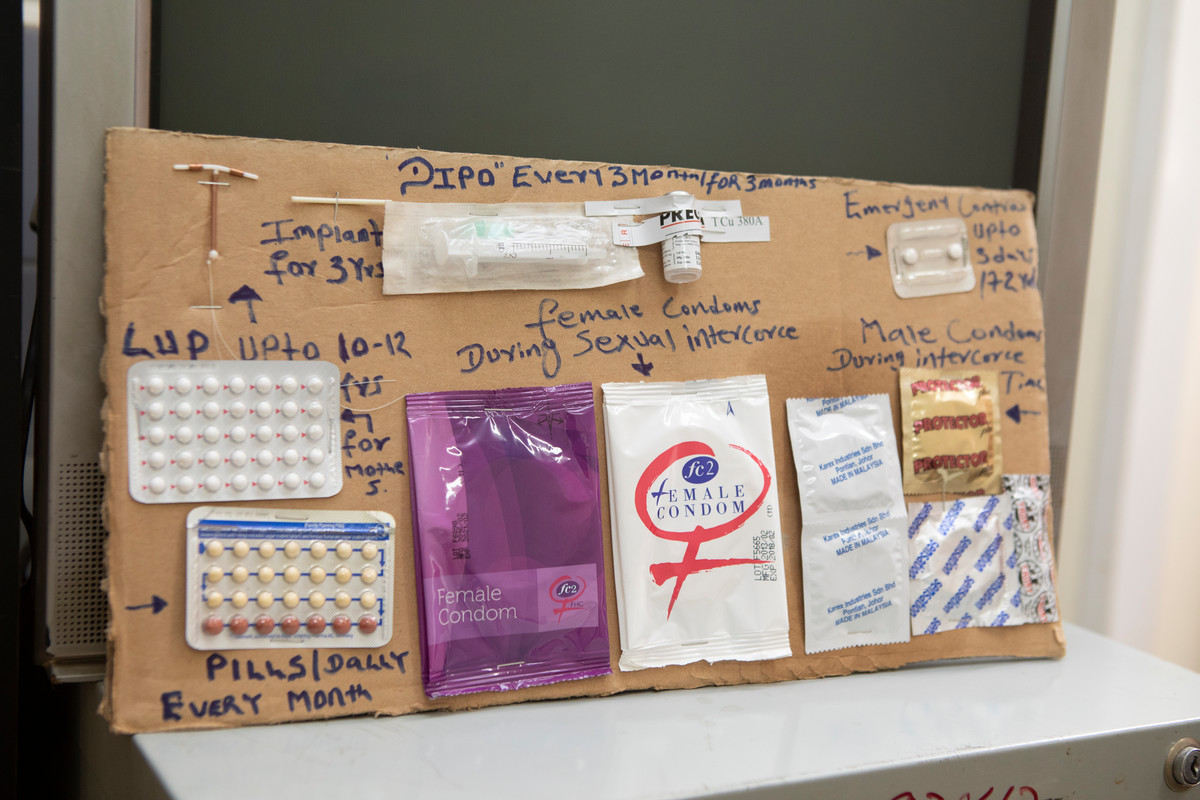
There is always some giggling when the group’s leader, 24-year-old engineering student Tsegay Teklehaimanot, shows how to use male and female condoms.
“They laugh and they love it,” he said.
The club has more than a thousand members and the work the peer educators do is voluntary, but rewarding.
“I’m proud of doing that thing because I am educating my friends and my family and protecting them,” says Teklehaimanot.
Biology student Gebre Haileselassie says that young people will discuss things with their peers that they would be embarrassed to ask their parents.
“In this place, we talk easily and are happy to talk,” he said.
“The main message and point is how to protect ourselves, because in our world now, there are a lot of diseases and infections,” he said.
The peer educators often stress the risks involved with drinking and having unprotected sex, especially with strangers.
“There are so many students that don’t know how to use condoms and [what to do] if something happens,” said Teklehaimanot.
Unintended pregnancies often mean female students drop out of school, and most are not aware of other options, so the peer educators provide information and refer them to counselling services.
Unsafe abortion numbers drop

Baraki has been working at the main FGAE clinic in Mekelle for 21 years and seen the number of unsafe abortions performed by traditional healers drop in recent years, and the number of young people coming in for comprehensive abortion care rise.
“Especially in high schools and universities it has increased,” she said.
“Nowadays awareness is increasing, especially in post-abortion complications and use of contraceptives,” she said.
Complications arise due to traditional healers inserting sharp, unsterile instruments into the uterus or prescribing a concoction of antibiotics, toxic tree leaves and strenuous exercise.
In rural villages however, Baraki has seen the number of safe abortion decrease “due to some changing norms”, she says, although outreach services have also dropped due to budget cuts.
Contraceptive shortages in rural areas
Programs to help youth in rural areas have been scaled back in recent years due to a decrease in funding for SRH services from international donors and the government of Ethiopia. Mekelle had to cut its monthly visits to twelve rural districts in Tigray to once a quarter, then completely, and other partners have also stopped doing outreach in rural areas.
“Nowadays they are not there and these services that are given by them are not supported now,” said Abadi.
The cuts also mean that in Tigray, there are shortages of condoms and HIV testing kits, including at the youth center.
Thanks to an FGAE program to provide free SRH services and products through public and private clinics, many young people and the poor from rural areas that come to Mekelle to sell produce now go to a 24-hour private clinic located in downtown Mekelle.
Clinic owner Temegen Weldegiorgis says that many students come to get contraceptives, STI testing and comprehensive abortion care here because they can’t afford to pay for services, but fear being seen by family members at public clinics.
The clinic serves a lot of teenagers who know nothing about family planning and the risk of STIs, and other underserved or unreached groups that need a drop in service in the center of town, such as farmers, sex workers, people living with a disability and veterans.
“They need privacy and so come and have the service here,” he said.